Learn About Protein & CKD
Kidneys filter excess protein in our blood. When you have chronic kidney disease, additional filtering can cause even more damage to the kidneys. Plant-based eating patterns have been shown to prevent the progression of kidney disease. This guide breaks down how kidneys process protein, how much and which types of protein are best for CKD, and ways to optimize your protein intake.
What is protein, and how does it affect kidneys?
Protein is one of the three ways we get energy from food. The protein in the food we eat is broken down and used as fuel for our bodies or helps build/maintain muscles and other body tissues. Protein is different from the other energy sources (carbohydrate and fat) as it contains nitrogen in its structure. During digestion, protein is broken down into individual units called amino acids. Then the nitrogen in protein is stripped, used to make new proteins, or made into urea and eventually removed from the body in urine. Urea is the waste product of extra nitrogen in the blood. Healthy kidneys can filter out extra urea in the blood and remove it in the urine.[1]
We can use the blood urea nitrogen (BUN) lab test to evaluate kidney function. When BUN is elevated, it can be a sign that the kidneys are not working properly. Creatinine is another blood test that is used to evaluate kidney function. While creatinine is also related to protein; it is reflective of muscle turnover in our bodies and is not as strongly linked to recent diet intake.[2] The build-up of these protein waste products is called uremia.[3] Uremia can occur slowly over time as in Chronic Kidney Disease (CKD) or quickly as in Acute Kidney Injury (AKI). During CKD, the slow build-up often goes unnoticed until a blood test indicates a high value. AKI, however, is usually a result of a severe injury or illness. People with AKI may regain kidney function, or the kidneys may not function as well as before.
Signs and symptoms of uremia include; fatigue, muscle cramps, mental confusion, loss of appetite, nausea and vomiting, fluid build-up or edema, itching, and unintentional weight loss.
When kidneys are not working properly, protein can also leak into urine. Often doctors will evaluate both blood and urine samples to assess kidney function and risk. In 2012, KDIGO (Kidney Disease Improving Global Outcomes) developed the table below that shows the potential risk for progression of kidney disease.[4]
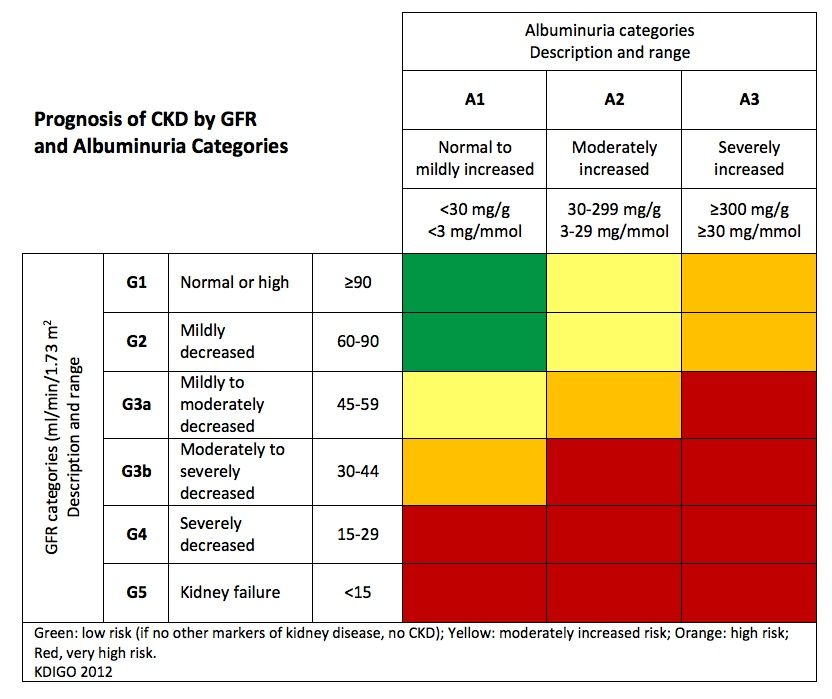
Chronic Kidney Disease healthcare teams utilize medications, lifestyle, and diet changes to maintain kidney function and prevent proteinuria (protein in the urine). One key aspect of this plan is to eat the correct amount of protein for the stage of kidney disease.
How much protein do I need for kidney health?
The goal for kidney health with CKD is to eat the right amount of protein to stay healthy but not so much as to cause the kidneys to be overworked and have protein leak into the urine. Eating the appropriate amount of protein for your stage of kidney disease is a way to maintain balance. Below are the clinical practice guidelines for protein. [5]
CKD Stage 1-2
0.8-1.0 grams protein per kg body weight
CKD Stage 3-5
Non-diabetic 0.55- 0.6 grams protein per kg body weight
Diabetic 0.6-0.8 grams protein per kg body weight
Dialysis
1.0-1.2 grams of protein per kg body weight
Example of how much protein is required for a person who weighs 160 pounds:
- CKD Stage 1-2: 58- 73 grams of protein a day
- CKD Stage 3-5: 44- 58 grams of protein a day
- Dialysis: On dialysis 73- 87 grams of protein a day
Sometimes people follow a stricter protein restriction of 0.28- 0.43 g/kg BW with the addition of a keto analog supplement. This level of protein restriction should only be done in people who are considered stable and with their doctor’s approval.
Understanding exactly how to meet and not exceed guidelines for protein can be difficult. Renal Dietitians, support and educate people with kidney disease.
Foods high in protein
Protein is typically associated with animal meat (chicken, eggs, fish, beef, pork, shellfish etc) however, there is also protein in legumes, nuts, beans, peas, pasta, tofu etc. Depending on how much protein you need in a day, you may need to be aware of the “typical” animal protein sources and the plant protein sources from foods like vegetables.
As mentioned above, individuals with CKD stages 3-5 should be limiting protein daily. Understanding how much protein is in food is a very good way to make healthy choices when putting food on your plate. Below is a table that includes protein in grams per serving. These are “typical” amounts, and it should be noted that individually processed foods such as yogurts may have variable grams of protein per serving.
Animal Protein Sources
- Ground Beef (3 ounces) 20g
- Steak (3 ounces) 21g
- Brisket (3 ounces) 18g
- Chicken drumstick (1 each) 13g
- Chicken Breast (3 ounce) 24g
- Chicken thigh (1 each) 28g
- Tuna (3 ounce) 22g
- Salmon (3 ounce) 20g
- Shrimp (3 ounce) 20g
- Pork Loin (3 ounce) 22g
- Pork Chop (3 ounce) 20g
- Milk, 2% (½ cup) 4g
- Cottage Cheese (4 ounce) 14g
- Yogurt (6 ounce) 6g
- Yogurt, greek (6 ounce) 16g
- Cheese, Mozzarella (½ cup) 12g
- Cheese, Swiss (1 oz slice) 8g
- Cheese, Cheddar (1 oz slice) 7g
- Egg (1 whole) 6g
Plant Protein Sources
- Beans (½ cup) 7g
- Lentils (½ cup) 9g
- Tofu (½ cup) 9g
- Nuts (¼ cup) 6g
- Sunflower seeds (1 ounce) 5g
- Rice Milk (1 cup) 1g
- Soy Milk (1 cup) 6g
- Yogurt, Coconut (6 ounces) 1g
- Tempeh (3 ounce) 16g
- Peanut Butter (2 Tbsp)
- Hummus (2 Tbsp) 8 g
- Bread, wheat (1 slice) 3 g
- Bagel (1 each) 10g
- Brown Rice (½ cup) 3g
- Wild Rice (½ cup) 4g
- Quinoa (½ cup) 8g
- Pasta (½ cup) 8g
- Cauliflower (½ cup) 2g
- Peas (½ cup) 4g [6]
Animal versus plant protein
Plant-based eating patterns have become a hot topic in research and the diet world. Plant-based diets focus on fruits, vegetables, legumes, nuts, seeds, whole grains, healthy fats, and beans. Sometimes people choose not to eat any animal products, and other times, the diet is focused on whole plant foods with fewer quantities of meat. An example of plant-based diets that have been shown to slow the progression of CKD include; whole-food plant-based (7), vegetarian(8), DASH [9], and the Mediterranean diet. [10] These diets all prioritize whole foods and minimize or eliminate the use of processed foods.
The kidneys handle animal protein differently than plant protein. A study showed that healthy people eating an animal protein-based diet had kidney hyperfiltration compared to a diet of vegetable-based protein. [11] Hyperfiltration is when the kidneys increase the filtering of blood (GFR). Hyperfiltration often happens during pre-kidney disease states but can indicate a risk for developing proteinuria (protein in the urine) and CKD. [12]
Plant-based proteins allow people to meet their protein requirements while feeling full at the end of a meal. Studies have shown that eating >50% of protein from plant-based sources reduces the progression of CKD. [13]
Plant-based sources of protein are less acidic than animal-based sources. One of the roles of kidneys is to support acid/base balance in the blood. Following a diet higher in fruits and vegetables and lower in red meats/processed foods has been shown to support acid/base balance in CKD. [ 7, 10]
Plant-based eating patterns have more beneficial effects than just kidney-protective kidney health. These eating patterns are also typically higher in fiber, antioxidants, vitamins, minerals, and antioxidants to support heart health, diabetes, gut health, obesity, and inflammation. [13]
Ways to limit protein
If you are someone whose kidney disease is stage 3-5 non-dialysis, you will need to limit the amount of protein you eat in a day. It can be very hard in a culture that focuses on meal planning around what meat is being served. There are ways to limit your protein intake and still enjoy meals.
Start by adding vegetables and fruits to your dinner plate first.
- Fill your plate with vegetables and fruit first (don’t forget to eat them first, too).
- Then add carbohydrates like brown rice, farro, pasta, and protein sources to help limit the total protein you serve yourself.
- Lastly include, healthy fats like those in olive oil, avocados, and nuts in moderation will keep you full and prevent weight loss on a low protein diet.
Limit portion sizes of protein.
Understanding how much protein is in a food serving helps you decide how much can be added to meet nutritional needs.
Typical serving sizes:
- ½ cup for beans/legumes- 7 grams of protein
- ¼ cup nuts- 6 grams of protein
- 6 ounces of yogurt- 1g to 15g of protein (variable based on product)
- 3 ounces or less of meat (fish, chicken, etc.)- 20 to 24 grams of protein
Add protein to soups, salads, and bowls as a garnish on top only.
Try a new plant-based meal weekly and build new food choices over time.
Choose plant-based meals for whole days at a time (for example, Meatless Monday) or 2 out of 3 meals per day.
Check out our Guide on the Plant-Based Diet for more ways to make meals delicious and kidney-friendly.
Ways To Increase Protein
If you are on dialysis, you have been told to add protein to your diet. When on dialysis, the focus of therapy changes from preserving kidney function to optimizing nutrition status and other health conditions (such as heart health and diabetes). Dialysis removes extra nutrients from the blood. Included in this removal is a protein in the blood called albumin. . Eating more protein in the diet compensates for the albumin protein that is filtered out in dialysis. [14] Below are ideas for increasing protein intake and still meeting your Renal Diet recommendations.
Make sure to incorporate a protein source at each meal and snack.
For example, do not settle for simple oatmeal. Add ¼ cup of nuts and blueberries to increase protein.
Do not be afraid to try plant-based protein sources.
Try new meals and protein sources to increase variety in your meals.
Add a protein supplement.
Try a protein supplement that meets your protein, phosphorus, and potassium needs.
Take medications as prescribed.
Take phosphorus binders or other prescribed medications to help support your kidney health.
Summary
Protein needs are individualized based on CKD stage and nutritional status. Limiting protein is a significant part of maintaining kidney health prior to end-stage kidney disease (dialysis). Studies continue to show that eating patterns based on plant-based foods support kidney health. Figuring out how much protein is suitable for you may be difficult; however, finding a renal dietitian to help individualize and support you in your kidney health can prevent the progression of CKD.

