Learn About Phosphorus & CKD
Phosphorus is a necessary mineral primarily found alongside calcium in the bones and teeth. In addition to bone health, it is an electrolyte and a necessary component of cell walls, RNA, DNA, and the body’s primary energy molecule (ATP). [1] Excess phosphorus in the body is filtered and removed predominantly by the kidneys, so people with kidney disease risk high phosphorus levels. High phosphorus levels are associated with a higher risk of chronic kidney disease progression, bone disease, and the development of hard calcifications in the heart and arteries. [2]
The normal phosphorus blood serum level for adults is 2.5–4.5 mg/dl. [1] Along with dietary restriction, high phosphorus management might also include phosphate binder medications and dialysis, depending on your stage of kidney disease. There are different forms of phosphorus in foods, some found naturally, and some found as additives in processed foods. An eating pattern that considers both nutrient density and phosphorus absorption is more beneficial for someone with kidney disease versus efforts to strictly limit the total phosphorus consumed in a day.
High Phosphorus Management
In people without kidney disease, the kidneys can excrete enough excess phosphorus to balance intake. As the glomerular filtration rate (GFR) declines, the amount of phosphorus the kidneys excrete out of the body through urine will eventually decline. [3]
Most people in the earlier stages of kidney disease will not have to use phosphorus lowering therapies to maintain normal blood levels. In contrast, most people in the later stages of kidney disease might require multiple therapies. The recommendation for people with CKD Stages 3-5D recommends lowering elevated phosphorus levels toward the normal range, reserving phosphate-lowering treatments to treat progressively or persistently high blood phosphorus levels. [4]
Three primary therapies help manage high phosphorus levels for people with chronic kidney disease:
- Dialysis for those with End-Stage Renal Disease
- Phosphate binder medications
- Dietary restriction
Dialysis for those with End-Stage Renal Disease
In Chronic Kidney Disease Stage 5D (also referred to as End-Stage Renal Disease -ESRD), the kidneys cannot function adequately to sustain life. At this point, there is minimal phosphorus excretion through the kidneys. Instead, dialysis filters the blood and has become one of the primary phosphorus management tools.
Depending on the duration and type of dialysis treatment, about 2100-3000 mg of phosphorus can be removed per week. [5] If you are on dialysis, your treatments significantly impact your phosphorus levels. Missed or shortened treatments can cause high phosphorus levels regardless of whether you are following a low phosphorus diet.
Phosphate (phosphorus) binder medications
Most people will not require a phosphate binder until late-stage kidney disease or ESRD. Still, when remaining kidney function and dietary restriction cannot maintain phosphorus levels within the normal range, a phosphate binder medication should be prescribed. [6] In 2021, about 80% of people receiving hemodialysis took a phosphate binder medication. [7]
A phosphate binder is a medication taken with meals and snacks to decrease the absorption of phosphorus from the foods you eat. These medications work by “attaching” to some of the phosphorus in your food and making a molecule that can’t be absorbed into the bloodstream. [8]
If you are prescribed a phosphate binder, it is incredibly important for you to take them as prescribed when you eat to protect your body from damage related to high phosphorus levels.
Common phosphate binder medications: [9]
- Calcium acetate (Phoslo)
- Calcium carbonate
- Ferric citrate (Auryxia)
- Lanthanum carbonate (Fosrenol)
- Magnesium/calcium carbonate
- Sevelamer carbonate (Renvela)
- Sevelamer hydrochloride (Renagel)
- Sucroferric oxyhydroxide (Velphoro)
Dietary restriction
Limiting phosphorus in the diet might seem straightforward, however, limiting total daily phosphorus without regard to the source hasn’t been shown to improve health outcomes. It actually has the potential to compromise adequate intake of other nutrients. [4]
The amount of phosphorus that is absorbed into the bloodstream that impacts blood levels will depend not just on the total amount of phosphorus in food but also on the bioavailability of that phosphorus in the food. [10]
What does bioavailability mean? It is the percentage of a nutrient in a food that will actually be absorbed and can be utilized in the body. [11]
Some of the factors impacting phosphorus bioavailability can include the following: [11]
- The structure of the food containing phosphorus
- The chemical form of the phosphorus in the food
- Interactions between various nutrients and phosphorus
- Processing and cooking method of the food
Through the interplay of these factors above, the typical “Western” diet, which is high in both animal-based and processed foods, appears to create an optimal intestinal environment for a high rate of phosphorus absorption. [10]
The remainder of this article will focus on recommendations to best manage phosphorus found in plant-based foods, animal-based foods, and processed foods based on their phosphorus bioavailability and total nutrient density.
Foods High in Phosphorus
Overview of Foods High in Phosphorus
Beverages
- beer/ale
- chocolate drinks
- cocoa
- dark colas
- drinks made with milk
- canned iced teas
- pepper type soda (Dr. Pepper)
- bottled beverages with phosphate additives
Dairy Products
- cheese
- liquid non-dairy creamer
- custard
- ice cream
- milk
- pudding
- cream soups
- yogurt (Greek type acceptable)
Protein
- oysters
- sardines
- beef liver
- chicken liver
- fish roe
- organ meats
Other
- chocolate candy
- caramels
- oat bran muffin
- most processed/prepared foods
- pizza
- brewer’s yeast
Plant-based foods naturally high in phosphorus
Plant-based phosphorus bioavailability is much lower compared to the amount of phosphorus in the food. Phosphorus naturally present in foods is often bound to proteins. This means the body needs special enzymes to break the protein bonds before phosphorus can be absorbed. Additionally, phosphorus in plants is mostly in the form of phytate which is compound humans poorly digest. [12] Because of both of these factors, the bioavailability of phosphorus from plant-based foods is relatively low even if they have a high phosphorus content.
It’s estimated that <50% of the phosphorus naturally present in plant-based foods can be absorbed. [5] For example, a half-cup of almonds contains 344 mg phosphorus, but only about 172 mg can be absorbed. [13]
Plant-based foods highest in phosphorus include




These foods also contain protein and are high in fiber, vitamins, and other minerals making them great choices to incorporate into a kidney healthy diet.
In general, it does not appear beneficial to limit these plant-based foods in order to manage high phosphorus levels. [14]
Animal-based foods naturally high in phosphorus
Repeating from above, phosphorus naturally present in animal-based foods is often bound to proteins, requiring protein enzymes and digestion time before phosphorus can be absorbed. Animal foods do not, however, contain phytate so their phosphorus absorption rate will be higher than plant-based foods. [15] Estimates for absorption of naturally occurring phosphorus in animal-based foods are 40%–70%. [1] There is evidence that suggests utilizing plant vs animal-based proteins might have beneficial impacts on phosphorus outcomes. [15]
According to the 2015-2016 National Health and Nutrition Examination Survey (NHANES), The top five sources of total and naturally occurring phosphorus, representing approximately 20% of intake, were cheese, pizza, chicken, reduced-fat milk, and eggs/omelets. [16]
Below are some practical tips for managing phosphorus found naturally in animal-based foods:
1: Consider Limiting Your Intake of Foods that Contain Dairy
Example: can you decrease dairy foods to once daily or switch to plant-based alternatives?
2: Reduce Your Portion Sizes of Animal-based Proteins*
Example: can you limit animal protein portions to 3 oz or less?
3: Substitute Plant-based for Animal-Based Proteins*
Example: can you make a black bean patty instead of a beef patty for a burger?
4: Boil Animal Proteins to Reduce phosphorus content
Example: boiling and then draining sliced meat for 30 minutes reduced phosphorus content by 50%. [5]
*It will be important to still meet your protein needs so work with a kidney dietitian to know how much protein is right for you and your stage of kidney disease.
Foods with phosphorus added in processing (phosphate additives)
The prevalence and consumption of foods with phosphate additives have increased in recent decades. Phosphate additives are added to foods to preserve colors, maintain moisture, improve flavor, homogenize ingredients, and stabilize proteins. [17]
In contrast to naturally occurring phosphorus, phosphorus added to food in processing is generally found in molecules with only one chemical bond to break, making it very easily digested and quickly absorbed. We estimate that >90% of phosphorus in this form is absorbed into the bloodstream. [5]
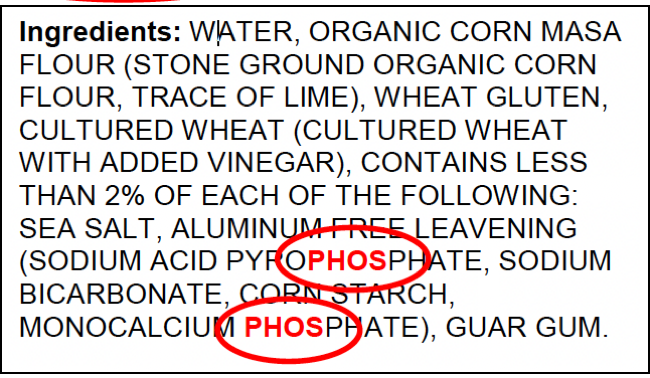
Phosphorus content is not currently required on U.S. food labels, but if phosphate additives have been used in the food, they must be listed in the ingredients list. [1]
Examples of phosphate additives you might find include the following:
| Dicalcium phosphate | Hexametaphosphate |
| Disodium phosphate | Dicalcium phosphate |
| Monosodium phosphate | Ferric phosphate |
| Phosphoric acid | Sodium phosphate |
| Sodium hexameta-phosphate | Monocalcium phosphate |
| Trisodium phosphate | Aluminum phosphate |
| Tetrasodium pyrophosphate | Sodium polyphosphate |
| Tetrasodium phosphate | Sodium tripolyphosphate |
| Phosphoric acid | Pyrophosphate polyphosphate |
Below is a table of the top sources of added phosphorus according to the 2015-2016 NHANES: [16]
| Food | % of daily intake in US adults |
| Cheese | 14.95 |
| Soft drinks | 9.36 |
| Cakes and pies | 9.15 |
| Rolls and buns | 6.08 |
| Cookies and brownies | 5.98 |
| Doughnuts, sweet rolls, pastries | 5.77 |
| Tortillas | 5.67 |
| Diet soft drinks | 5.37 |
| Cold cuts and cured meats | 4.51 |
| Chicken, whole pieces | 4.27 |
| Yeast breads | 3.58 |
| Biscuits, muffins, quick breads | 3.30 |
| Nutritional beverages | 3.16 |
| Cream and cream substitutes | 2.81 |
| Pancakes, waffles, French toast | 2.59 |
Placing the bulk of dietary phosphorus restriction on phosphate additives appears to have the greatest impact on outcomes without compromising the nutrient content of the diet. [12,17]
Based on all of this information, here are some practical tips for managing phosphorus added to foods in processing:
- Read ALL your food labels for ingredients that include the letters “phos” and switch to an alternative without phosphate additives. Example: instead of eating a granola bar with monocalcium phosphate in the ingredients, choose another without phosphate additives.
- Cook from fresh/scratch as much as you can. Prepackaged and processed foods will always contain more easily absorbed phosphate additives than something prepared from scratch. Example: Make your own vinaigrette instead of using ranch dressing with dicalcium phosphate.
- Limit fast food. Most fast-food restaurants rely heavily on phosphate additives to maintain the quality and convenience of their foods. Example: Make your own breakfast sandwich at home instead of having a fast-food breakfast sandwich and you could save 200-300 mg of phosphorus. [18]
- If you eat cheese or products with cheese, choose “natural” over “processed.” Example: Choose natural cheese like cheddar instead of American cheese processed with tricalcium phosphate.
- Watch out for processed and enhanced meats. Deli meats, cold cuts, and enhanced fresh meats can be a significant source of phosphorus in the diet. [19] Example: choose to make a vegetarian sandwich or a sandwich with fresh chicken breast vs cold cuts.
- Check your beverages. If you can, choose water. Sports drinks, powdered drink mixes, cola drinks, bottled teas, and milk (both dairy and plant-based) beverages often have phosphate additives. Example: have some water with lemon or homemade lemonade instead of powdered lemonade mixed with sodium acid pyrophosphate.
Summary
By reading this article you know that high phosphorus levels cause significant risk to health and dietary restriction is one of a few therapies used to manage phosphorus in CKD.
Research shows that adherence to dietary patterns rich in fruit and vegetables, fish, legumes, cereals, whole grains, and fiber, and lower in red meat and products containing sodium and refined sugars is associated with lower mortality in people with CKD. [14] By following this type of eating pattern, most people will already significantly reduce their phosphorus intake because they are choosing foods that have lower phosphorus content and bioavailability.
If you need more guidance implementing low phosphorus or other CKD diet recommendations, seek out a renal or kidney dietitian!
References
- NIH. (2021). Office of Dietary Supplements – Phosphorus. Nih.gov. https://ods.od.nih.gov/factsheets/Phosphorus-HealthProfessional/
- Nadkarni, G. N., & Uribarri, J. (2014). Phosphorus and the kidney: What is known and what is needed. Advances in nutrition (Bethesda, Md.), 5(1), 98–103. https://doi.org/10.3945/an.113.004655
- Blaine, J., Chonchol, M., & Levi, M. (2015). Renal control of calcium, phosphate, and magnesium homeostasis. Clinical journal of the American Society of Nephrology : CJASN, 10(7), 1257–1272. https://doi.org/10.2215/CJN.09750913
- Ketteler, M., Block, G. A., Evenepoel, P., Fukagawa, M., Herzog, C. A., McCann, L., Moe, S. M., Shroff, R., Tonelli, M. A., Toussaint, N. D., Vervloet, M. G., & Leonard, M. B. (2017). Executive summary of the 2017 KDIGO Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD) Guideline Update: what’s changed and why it matters. Kidney international, 92(1), 26–36. https://doi.org/10.1016/j.kint.2017.04.006
- Barreto, F. C., Barreto, D. V., Massy, Z. A., & Drüeke, T. B. (2019). Strategies for Phosphate Control in Patients With CKD. Kidney international reports, 4(8), 1043–1056. https://doi.org/10.1016/j.ekir.2019.06.002
- Isakova, T., Nickolas, T. L., Denburg, M., Yarlagadda, S., Weiner, D. E., Gutiérrez, O. M., Bansal, V., Rosas, S. E., Nigwekar, S., Yee, J., & Kramer, H. (2017). KDOQI US Commentary on the 2017 KDIGO Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). American journal of kidney diseases : the official journal of the National Kidney Foundation, 70(6), 737–751. https://doi.org/10.1053/j.ajkd.2017.07.019
- Mineral and Bone Disorder- Phosphate binder use, last 3 months. DOPPS Practice Monitor . Retrieved April 22, 2022, from https://www.dopps.org/DPM-HD/DPMSlideBrowser.aspx?type=Topic&id=11
- Council on Renal Nutrition (Ed.). (2022, February 25). Phosphorus and your diet. National Kidney Foundation. Retrieved April 22, 2022, from https://www.kidney.org/atoz/content/phosphorus#what-medications-are-phosphorus-control
- Marr T. (2009). Nutrition in Kidney Disease, edited by Laura D. Byham-Gray, Jerrilynn D. Burrowes, and Glenn M. Chertow. Proceedings (Baylor University. Medical Center), 22(2), 161.
- Saurette, M., & Alexander, R. T. (2019). Intestinal phosphate absorption: The paracellular pathway predominates?. Experimental biology and medicine (Maywood, N.J.), 244(8), 646–654. https://doi.org/10.1177/1535370219831220
- Ostrenga, S. (2018, January 30). Are you absorbing the nutrients you eat? MSU Extension. Retrieved April 24, 2022, from https://www.canr.msu.edu/news/are_you_absorbing_the_nutrients_you_eat
- Fukagawa, M., Komaba, H., & Miyamoto, K. (2011). Source matters: from phosphorus load to bioavailability. Clinical journal of the American Society of Nephrology : CJASN, 6(2), 239–240. https://doi.org/10.2215/CJN.11051210
- U.S. Department of Agriculture. (2019, April 1). Nuts, almonds. FoodData Central. Retrieved April 24, 2022, from https://fdc.nal.usda.gov/fdc-app.html#/food-details/170567/nutrients
- Kelly, Jaimon T et al. “Healthy Dietary Patterns and Risk of Mortality and ESRD in CKD: A Meta-Analysis of Cohort Studies.” Clinical journal of the American Society of Nephrology : CJASN vol. 12,2 (2017): 272-279. doi:10.2215/CJN.06190616
- Moe, S. M., Zidehsarai, M. P., Chambers, M. A., Jackman, L. A., Radcliffe, J. S., Trevino, L. L., Donahue, S. E., & Asplin, J. R. (2011). Vegetarian compared with meat dietary protein source and phosphorus homeostasis in chronic kidney disease. Clinical journal of the American Society of Nephrology : CJASN, 6(2), 257–264. https://doi.org/10.2215/CJN.05040610
- Fulgoni K, Fulgoni VL 3rd. Trends in Total, Added, and Natural Phosphorus Intake in Adult Americans, NHANES 1988-1994 to NHANES 2015-2016. Nutrients. 2021 Jun 29;13(7):2249. doi: 10.3390/nu13072249. PMID: 34210102; PMCID: PMC8308364.
- de Fornasari, M. L., & Dos Santos Sens, Y. A. (2017). Replacing Phosphorus-Containing Food Additives With Foods Without Additives Reduces Phosphatemia in End-Stage Renal Disease Patients: A Randomized Clinical Trial. Journal of renal nutrition : the official journal of the Council on Renal Nutrition of the National Kidney Foundation, 27(2), 97–105. https://doi.org/10.1053/j.jrn.2016.08.009
- Sherman, R. A., & Mehta, O. (2009). Phosphorus and potassium content of enhanced meat and poultry products: implications for patients who receive dialysis. Clinical journal of the American Society of Nephrology : CJASN, 4(8), 1370–1373. https://doi.org/10.2215/CJN.02830409
- U.S. Department of Agriculture. (2020, October 30). Egg, cheese, and bacon on biscuit. Retrieved April 24, 2022, from https://fdc.nal.usda.gov/fdc-app.html#/food-details/1100325/nutrients

